Ochsner’s (Southeast Louisiana) opioid stewardship efforts began in 2015. According to Todd Burstain, MD, the CMIO at Ochsner Health System, “Our approach to patient education and outreach started with some posters about narcotic use in our emergency department and clinics. Those didn’t really move the needle, though. We realized that effective outreach and education required a solid foundation of analytics and reporting.
Two of our top priorities were to 1) accurately separate chronic opioid users from acute opioid users, and 2) identify which chronic patients might be at risk for opioid misuse.”
Ochsner built a chronic opioid registry and implemented a customized Opioid Risk Tool. Chronic opioid patients were categorized as either “high” risk, “medium” risk, or “low” risk, based on factors such as frequent early refill requests, recent dose escalations, as well as factors related to social and family history.
Burstain points out, “Knowing our chronic opioid patients’ level of risk was critical, but we also wanted to take the next step and actually monitor – and engage – those patients.”
After sitting down with a team of experts, Ochsner established specific requirements for chronic opioid patients depending on their risk level, managed through the Health Maintenance section in Epic (see rules below). Importantly, these tasks were also pushed to the patient portal. Per Burstain: “So when one of our chronic opioid patients logs into Epic MyChart, they might see they are overdue for a mammography or colonoscopy, and right there alongside that information is a reminder that we would like them to sign a pain contract, or an alert that they need to refill their Naloxone prescription.”
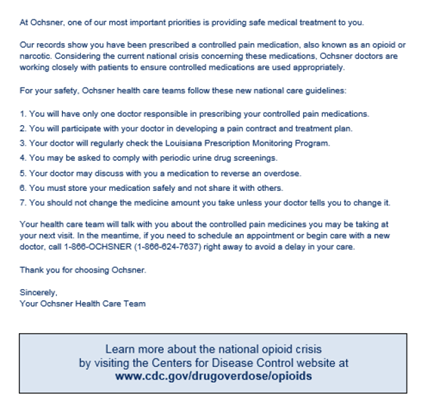
After the registry was created, Ochsner also crafted a letter to all of their chronic opioid patients (see sample below). The letter included background on the opioid epidemic, outlined the patient’s specific care plan and risk level – and most importantly, emphasized that Ochsner’s top priority was to provide them with the safest care possible. According to Burstain, “We found that our patients were extremely grateful for our outreach efforts. One of the most common responses we heard was ‘thank you – I had no idea that I was even at risk.’”
In terms of outreach and education to a broader patient population, Ochsner worked with local experts to create a do/don’t list for opioids. Any time an Ochsner patient is prescribed an opioid, that educational sheet is automatically included in the after-visit summary (both post-hospital discharge or after an outpatient visit). Additionally, any Ochsner patient with pain in his or her problem list is given access to related digital content through the patient portal.
Keys to Success:
- The right message. According to Burstain, “Patients need to know you are doing this because you care. It isn’t about some law or regulation – it is about their safety.”
- Help patients understand the risks. Even though most patients may be aware of the opioid crisis, they may not know the specific risks; how opioids may interact with other medications, the dangers of mixing opioids with alcohol, or the importance of storing their medications in a safe place.
- Explain the options. “There are a lot of alternatives to opioids that patients may not know about,” says Burstain. “For example, we are using virtual reality to help distract patients from the pain of certain procedures and minimize their initial exposure to opioids. It is critical that patients understand all of the options.”