Chapter 1 focused on strategies for creating an Opioid Stewardship Committee, with examples from an academic medical center, large healthcare systems and a critical access hospital. Based on the experience of these organizations and many other health systems, it’s safe to say that an Opioid Dashboard is one of the first deliverables that the Opioid Stewardship Committee will need. The dashboard will play a critical role as a tool to view and monitor performance metrics and present other relevant data. However, it is very important that the dashboard is delivered in partnership with the committee—not as a prerequisite to the creation of the committee. Many initiatives fail to launch while business intelligence teams toil at creating perfect dashboards without the input or buy-in of the initiative leaders.
This is not to say that the IT leader won’t do some homework leading up to the initial meeting of the Opioid Stewardship Committee. It is important for the informaticist to guide and ground the committee in what can be done using reasonable goals and measurements. Just as the medical directors should do literature review before heading into the meetings, the IT leaders should have a firm grasp on:
- What their vendors provide out of the box
- What their team has the ability to customize
- What technologies and metrics have been successful at other organizations
This chapter of the playbook will walk you through those considerations. But before you get started, you need a clear idea of your organizational goals for this initiative.
Setting a goal
Most of the organizations we surveyed had the following among their key goals:
Invest in the future health of our community by reducing the pipeline into addiction. This requires us to reduce the total Morphine Milligram Equivalents (MMEs) that are prescribed, especially for opioid naïve patients.
Whether your organization chooses this as one of its goals is up to the discretion of the committee. But let’s use this as an example.
In this case, you haven’t built a dashboard to try and dictate the goal. Instead, you’ve waited for your committee to set this goal first and offer further definitions of exactly what you should be measuring. In this example, we’re not just measuring the total MME, but we also want the ability to drill down on a subset of patients who are not yet addicted. Now that you have this definition, you can begin working on the reports and dashboards that will track this metric in lockstep with the actual effort of the committee.
Start Building
At some point fairly early in the effort, you’ll notice that you have a handful of working metric definitions that tie to the Stewardship Committee’s goals. It’s highly advisable to document these definitions so that users can easily understand what the dashboards are telling them. It also helps the credibility of the dashboard to know that the definitions were discussed and agreed among medical and operational leaders.
Now that you’ve got a working set of your first few metrics, it’s time to start building! Keep these high-level goals in mind:
- Measure your baselines
- Track progress
- Break down the progress to functional areas
- Do a strong wave of data validation with your operational counterparts
- Create the framework for your clinical leaders to have conversations with their teams
Key Insight
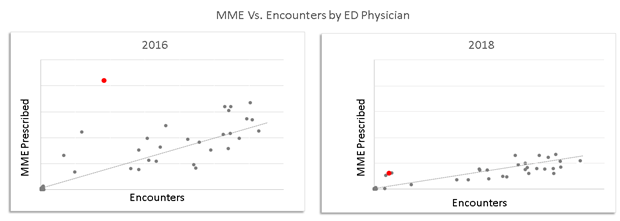
The ultimate way a dashboard drives change is by enabling conversations. Create a dashboard that allows medical directors to have a conversation with physicians about normal prescribing practices, outlier situations, and standard protocols. Without these conversations, change can’t happen.
A common practice among successful organizations we surveyed for this chapter was their dashboard was an ever-evolving work. New functionality was continuously added throughout the initiative. This meant when they first started, they were able to publish some initial data, make an operational change, publish new data, and continue the cycle until the dashboard and the initiative were mature. You may recognize this as a sort of “Agile development” method, where a small product is delivered initially and then improved until it becomes mature. This method appears to be common among dashboard builders who succeeded in their Opioid Reduction initiatives.
Governance
Just like most big initiatives, you will quickly encounter the situation where there are more good ideas than resources to build dashboards and technologies to support the ideas. That’s OK! It just needs to be well managed, and your experience as an IT leader has already given you the solution to this problem: Governance.
The teams we surveyed commonly had a process in place that allowed them to prioritize the ideas generated in the Stewardship Committee and rank them by the estimated opportunity. They also were able to specify to the committee how many IT FTEs were available for the initiative. These two inputs allowed the technology and operational teams to have the same set of expectations as they worked through the queue of ideas in priority order.