Most patients are acutely aware of the national opioid epidemic – whether being personally affected by an opioid-related tragedy or just seeing the chilling statistics on the news. This heightened awareness has made patient education more important than ever, though. There is now an expectation from patients and family members that hospitals will not only proactively provide education about opioids, but also will be able to address specific concerns and questions. The sheer amount of news coverage also means that some patients may have misconceptions about opioids – and pain management – that need to be dispelled. Technology increasingly plays a more prominent role in efforts to educate and engage patients about opioids, but it is still early – and IT-centric approaches are still evolving.
“Patients and family caregivers should receive real-time education at the time of initial prescription, prescription fulfillment, and on an ongoing basis. Patients and family caregivers also should be engaged in setting realistic pain management goals based on expectations for safe and effective pain relief and functional outcomes. Patients should know how to use opioids safely once they have left the healthcare setting, and thus the healthcare team must teach techniques for safe drug use, storage, and disposal, as well as signs of drug overdose, diversion, and opioid use disorder (OUD).”
Patient Education with Joint Decision Making and Treatment Agreements
Prescribers should engage patients in a conversation about their expectation for pain and options for management. This requires patient education. Education should include considerations that address biopsychosocial factors with pain care:
- Defining and understanding contributing factors associated with pain
- Education on types of pain and factors that can influence or impact pain
- Differentiation of pain management strategies for acute and persistent or chronic pain
- Education on treatment options including non-pharmacological alternative methods for reducing and managing pain
It is important for care team members to direct patients to credible sources of health information, as an uninformed patient can be easily misdirected by divergent and sometimes false information. (See the “Resources” section for a list of credible sources.)
Shared decision making and use of treatment agreements will assist providers to review realistic benefits, risks and side effects (both common and serious), as well as alterative treatment options with the patient (see Table 1). Health systems and hospitals must fully support providers in helping connect patients to resources, appropriate treatment, social support and the help they need.
Patient engagement and shared decision making requires:
- Discussing benefits, risks and side effects of opioid use, and providing clear and easy-to-understand educational materials
- Offering alternative pain management options
- Assisting patients to focus on managing acute pain during healing and improve functionality
- Discussing safe storage of opioid medications, including keeping out of reach of others
- Encouraging questions and providing follow-up opportunities
The Role of Technology in Patient Education
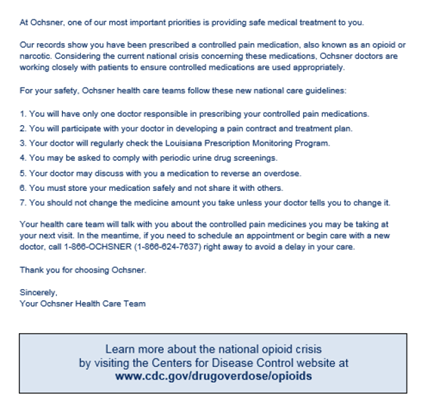
IT has proven to be an effective means for accurately identifying patients at risk for opioid misuse (see “Real World Examples” below). Technology is even increasingly playing a role in treating opioid use disorder (OUD); in fact, the first prescription digital therapeutic for patients with OUD was approved by the FDA in December 2018. When it comes to educating patients about the risks of opioids, though, approaches at most hospitals and health systems to date have been fairly “low tech” – focused primarily on paper handouts, printed discharge instructions and general content pushed to the patient portal.
However, technology is starting to play a more prominent role in efforts to educate and engage patients about opioids, especially as leading hospitals and health systems are beginning to approach chronic opioid use the same way they approach other chronic conditions. For example, organizations like Ochsner Health System have built and implemented a custom registry of chronic opioid patients to serve as the foundation for their targeted education and outreach efforts (see details in “Real World Example” below). Tools from enterprise EHR vendors are also maturing.
Moving forward, technology will play an even bigger role in helping to provide patients with personalized, easy to understand, clinically effective educational content about opioids at appropriate points in the patient journey (through multiple mediums and platforms).
For example:
- Using chronic disease outreach tools in novel ways to address opioid education
- Electronic alerts embedded in clinical workflows at defined points of care reminding clinicians to provide patients with educational materials about opioids and/or direct the patient to appropriate resources or services
- Automated point-of-care recommendations and suggestions to providers about specific educational content, resources and/or services based on a patient’s unique circumstances and risk level for opioid misuse
- Automatically pushing customized, patient-specific educational content about opioids and pain management to patients’ mobile devices
- Real-time integration of new types of interactive digital education into existing patient-facing apps and tools
- Tracking/monitoring which patients have received opioid education (including when, what type of content, etc.)
- Quantifying/measuring which types of educational content and engagement initiatives are most effective (or most valued by patients)